What is Lichen nitidus?
Lichen nitidus is rare, chronic skin condition which is characterized by asymptomatic, flat skin-colored papules or bumps on the skin, but it can also affect mucous membranes and nails. Lichen nitidus is usually present in children and young adults, but it can affect persons of any age. It can occur equally often in any race [1].
Causes
The exact cause of lichen nitidus is not known. It is believed that this condition appears as an immune response by T lymphocytes. It is also not known what causes the T lymphocytes to be activated [1,2].
Associated diseases
Some diseases are associated with lichen nitidus:
- Atopic dermatitis
- Lichen plannus
- Condyloma
- Amenorrhea
- Chron disease
- Down syndrome
- Juvenile chronic arthritis
- Congenital megacolon
- HIV infection
- Tuberculosis [1,5]
Clinical features of lichen nitidus
Symptoms of the skin
Lichen nitidus usually presents as bumpy skin eruption in localized areas. The typical areas affected are:
- Flexor parts of the forearms
- Back of the arms
- Genitalia
- Buttocks
- Chest
The typical papules are:
- 1-2 mm in diameter
- Round shaped
- Color: skin colored, yellowish, red-brown, violet
- In dark skinned people hypo- or hyperpigented
- Flat
- Shiny
- Scaly
- May appear as tiny blisters
- Often found on elbows and knees, might resemble psoriasis
- Can become itchy
Köbner sign- when lichen nitidus papules are arranged in a line with scratch marks.
In older patients palms and soles might be affected.
If lichen nitidus affects the mucosa of the mouth, the papules usually appear grey-white colored and can be localized on cheek mucosa, tongue and hard palate [2,3].

![]()
Symptoms of nails
In rare cases, lichen nitidus can affect nails. It is seen in around 10% of cases, mostly in adults. Typical changes in nails are:
- Pitting
- Longitudinal ridging
- Splitting of nail edges
- Rippling
- Redness of nailfold [3]
Clinical variants
Lichen nitidus can be present in different clinical variants. These include:
- Generalized- affecting large areas of the body
- Hemorrhagic- usually begins from the feet and around ankles, later progressing up the legs. In a few moths this form becomes generalized.
- Vesicular- usually affects palms with formation of small blisters (vesicles)
- Actinic form- seasonal, usually appears in sun exposed areas
- Keratoderma-resembles eczema; usually affects palms and soles
- Perforating- usually appears on hands and forearms and has papules with umbilication on the surface [3].

![]()
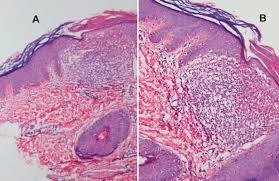
Diagnosis of lichen nitidus
The diagnosis is usually made by clinical examination and by histological examination of a skin biopsy material.
Histologically lichen nitidus is characterized by:
- Epidermis:
- Parakeratosis and atrophy
- Claw-like pattern of fingerlike extensions
- Sometimes multinuclear cells are seen
- Dermis:
- Infiltrations with lymphocytes and histocytes
- Dermoepidermal junction has variable dyskeratotic keratinocytes [4]
![]()
Differential diagnosis
The differential diagnosis of lichen nitidus includes several other skin disorders, such as:
- Lichen planus
- Lichen sclerosus, atrophicus
- Lichen spinulosus
- Lichen striatus
- Non-genital warts
- Sarcoidosis
- Psoriasis
- Bowenoid papulosis
- Keratosis pilaris [2,3]
- Cowden syndrome
Treatment
Usually lichen nitidus does not cause any symptoms therefore treatment is rarely necessary. for this reason, there hasn’t been any generalized studies to assess the best course of treatment. in most cases, this condition resolves on its own. In two-thirds of cases it resolves after 12 months. In some case the hyperpigmented areas of the skin can persist for months or years.
Treatment might be necessary for patients who present with generalized rash, itchiness, involvement of cosmetically sensitive sites and prolonged course of the disease. Treatment modalities that can be used are:
- Phototherapy:
- Psoralen plus UV-A light- penetrates deep levels of the skin. Usually used together with medications, that make the skin more sensitive to UVA rays.
- Narrow band UV-B light
- Sunlight exposure-can help to clear lichen nitidus, but patients should avoid sunlight for a few days after phototherapy.
- Topical corticosteroids– helpful in reducing inflammation process associated with lichen nitidus. However, the possible side effects should be weighed against the benefits. Side effects include:
- Thickening of skin in the used areas
- Lessening of treatment effectivity
- Oral corticosteroid long-term use can cause osteoporosis, diabetes, high blood pressure.
- Retinoids– synthetic A vitamin. Used both orally and topically. Topical retinoids can cause skin irritation. The use of oral retinoids can cause birth defects. They should be used with caution in women who are in fertile age or who are pregnant.
- Topical calcineurin inhibitors:
- Tacrolimus- works as an immune system suppressor.
- Side effects include: stinging, burning, itching
- Phototherapy and sunlight should be avoided when using these drugs
- Systemic cetirizine, levamisole, cyclosporine
- Selective H1 antagonists- antihistamines- oral or topical medication can relieve itching.
- Antibiotics- isoniazid [1,5]
Pictures




References
- General patient information: http://www.mayoclinic.org/diseases-conditions/lichen-nitidus/basics/definition/con-20028467
- General information for health specialists: http://emedicine.medscape.com/article/1123127-overview#a4
- Clinical features: https://www.dermnetnz.org/topics/lichen-nitidus
- Histology: http://pathologyoutlines.com/topic/skinnontumorlichennitidus.html
- Treatment: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2763760/