What is Testicular Torsion?
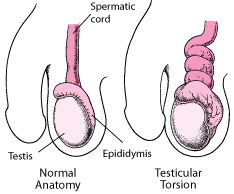
When the spermatic cord twists along with its contents, it may be referred to as testicular torsion. This is considered a surgical emergency to help correct the problem. Testicular torsion affects about 3.8 of every 100,000 males who are younger than 18 years every year, and in children it accounts for about 10 to 15 percent of all cases of acute scrotal disease. Again, testicular torsion contributes to a 42 percent orchiectomy rate (testicle removal rate) among boys who undergo surgery for detorsion.
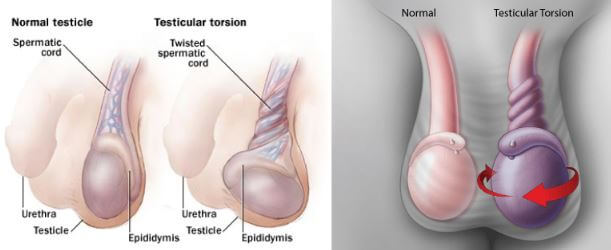
When it is identified that a person has testicular torsion, prompt treatment is needed to salvage the testicles. Torsion of the testicles will occur when the tissue surrounding the testicle does not attach properly causing the testes to curl around the spermatic cord. There is impaired blood flow when the twisting of the tissue occurs and it may cause pain as well as swelling.1,2,3,4,5,6
Symptoms
A person with testicular torsion will have sudden, severe pain that presents on one side of their scrotum. Usually, testes need to be of same size and when you see one side has become larger compared to the other, it may bring problems. Early on during testicular torsion, a person may not experience swelling but thereafter the scrotal skin swells and turns red.
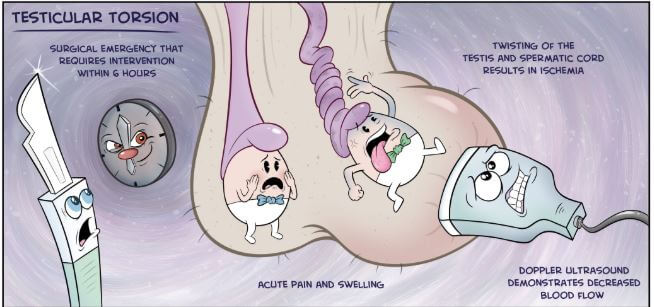
A person may also have the feeling of nausea and they may vomit. Because the blood entering the testicle goes through the spermatic cord, when the supply becomes cut off as a result of the twist, it may result in severe symptoms and a medical emergency is needed. The testicle shrinks, a situation known as atrophy if there is no restoration of the blood within 6 hours. If there is no blood feeding the testicles, they could actually die or become infarct. In the event that the testes die, then the scrotum becomes very tender and reddened. It’s also swollen.1,3,4,5
Other symptoms that may arise when you have testicular torsion include:
- Dizziness
- Lumps within the scrotal sac
- Presence of blood in semen
- Severe pain within the groin area
Since other conditions like epididymitis may cause testicular pain, it is important that a patient is examined by a doctor. Most often, the pain associated with testicular torsion occurs on side, and occurs mainly on the left. In most cases, symptoms such as problem with urination and frequent need to urinate, or a burning sensation are not associated with the condition.
Causes
Usually, there are two testes or testicles that hang within a pouch of skin and that pouch is known as scrotum and it sits below a person’s penis. It is in the testes where sperms and male sex hormone or testosterone are synthesized. Testicles are supplied blood by the spermatic cord that starts within the abdomen and runs into the scrotum. The bas deferens that transports sperm to the urethra from the testicles is also housed in the spermatic cord.1
When the tissue surrounding the testicle is well attached, you find that the testicle cannot twist, however, some individuals have a congenital condition where they are born without the tissue holding testes to scrotum. When this happens, it allows the tests to swing inside the pouch or scrotum, a condition referred to as bell clapper deformity.
Most people who have torsion of testes are born with increased risks of having the condition but they may not realize it. Usually, the testes cannot move freely inside the pouch and the surrounding tissue tends to be strong and supportive. When a male or boy has the bell clapper deformity where there is weaker connective tissue within the scrotum, it makes the testes to move much freely and it can increase the risk of twisting of the spermatic cord.
Other situations that may lead to testes torsion include:
- A male may have the condition following an injury within the groin area
- It may also be caused by rapid growth in time of puberty
- Sports injuries may cause the twisting of the cord
Torsion of testes can occur any time, while sleeping, standing, sitting, or exercising and without any apparent trigger, especially in those people who are susceptible.
If you are within the age of 10 to 25 years, you are more likely to have the condition. If you previously had it, then it could also happen again unless surgery has been performed. Sometimes, torsions are referred to as winter syndrome because they tend to happen during time of cold weather. When in bed, there is warmth and the scrotum is relaxed, but when the person leaves and walks in the room, the sudden exposure to cold air may bring about sudden contraction. If the cord was twisted when the individual was sleeping or when the scrotum was relaxed, upon exposure to sudden cold air, the testicle may become trapped in that twisted position leading to torsion.6
Diagnosis
Radiology
A doctor may physically examine the scrotum, abdomen, testes, and groin and ask questions regarding any symptoms a person may have. The doctor may rub or pinch inside the thigh within the affected side to test the reflexes. When there is testicular torsion, the reflex that causes testicles to contrast when you are pinched will not happen. In the event that a doctor cannot ascertain that it is torsion, a urologist is consulted immediately. This will help minimize any complications that may occur if treatment isn’t sought fast.
Medical tests
Medical tests that could help in confirming the condition include:
- Blood or urine tests that check for infection
- Nuclear scan of the individual’s testes – tiny amounts of radioactive substance are injected into the bloodstream to help detect areas where there is reduced blood flow.
- Scrotal ultrasound – this helps to assess the flow of blood. If there is reduced flow of blood, it could indicate torsion.
A doctor will most likely use ultrasound to evaluate the torsed testis. This imaging procedure is able to assess the testis structure and vascularity without inducing ionizing radiation to the gametes. During the examination, a doctor will compare the affected testis with the other one.7
A person may require exploratory surgery to help determine if the symptoms are as a result of torsion or some other condition. Even when surgery reveals no torsion has occurred, the surgeon may consider attaching the testis to the scrotum wall in order to prevent problems in future. Surgery will be performed if pain has persisted for several hours and a physical exam has suggested the possibility of torsion.
Treatment
Surgery
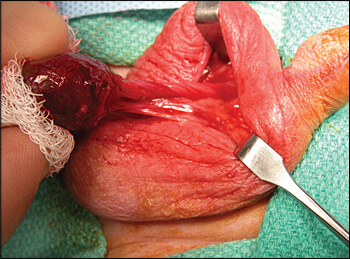
Surgery is the method of treatment of testicular torsion. When the surgery is done within 4 to 6 hours following the occurrence of the torsion, the testicle may be saved. However, if it takes longer, there may be permanent damage done to the tissue because of lack of blood supply. This may also affect ability of the person to father a child. The aim of the surgery is to untwist the cord to help blood to start flowing as usual and stitch or sew the testicle to the scrotum.
While manual detorsion may be done, surgery detorsion is recommended because it helps to prevent future occurrences of torsion. The operation is minimally invasive and very simple. The surgery is done under general anesthesia and usually it doesn’t require a person to remain in hospital. At time of surgery, a surgeon:
- Makes a cut right in the scrotum
- Untwists the spermatic cord
- Stitches the testis to the scrotum. Both testicles may be stitched to the scrotum to prevent torsion occurring within the other side.
Successful treatment is only possible if the testicle is untwisted within the shortest time possible following the torsion. If there is delay by more than 6 hours, there may be damage of tissue. After 12 hours, there is almost 75% likelihood of a person losing their testicle. If it happens that treatment hasn’t been done within 12 hours and the testicle is dead, then it may need to be removed in order to prevent gangrenous infection. One study examined that where surgery is delayed for more than 12 hours, then about 3 in 4 patients will require their testicle to be removed, a procedure known as orchidectomy or orchiectomy.
The surgical procedure to attach the testis to the scrotum may take about 45 minutes. Though there may be some pain, it isn’t as bad as that of torsion itself. If the testicle is to be removed, a procedure known as orchiectomy is applied.
After Surgery
A person will need to refrain from strenuous activities such as sports or sexual stimulation like masturbation at least for a couple of weeks following the torsion surgery. A patient may need to take some pain killer to help with pain. You may want to speak with your surgeon to find out how long it takes for you to get back to work. However, it may only take several weeks to recover from the surgery.
Prevention
Because there is inheritance of trait associated with testicle torsion, the best way to prevent the twisting from occurring is by having surgery that attaches both testicles to scrotum’s inside area to ensure there is no free rotation. Removing one testicle may not prevent someone from having children, but there may be reduced sperm count in people who have had surgery to remove a testicle.
Reference List
- What is Testicular Torsion? https://www.urologyhealth.org/urologic-conditions/testicular-torsion
- Testicular Torsion: Diagnosis, Evaluation, and Management. https://www.aafp.org/afp/2013/1215/p835.html
- Torsion of Testes. https://www.healthline.com/health/testicular-torsion
- Testicular torsion. https://www.mayoclinic.org/diseases-conditions/testicular-torsion/symptoms-causes/syc-20378270
- What Is Testicular Torsion? https://kidshealth.org/en/teens/torsion.html
- https://www.medicalnewstoday.com/articles/190514.php
- Testicular torsion. https://radiopaedia.org/articles/testicular-torsion